Iowa similar to US averages for economic costs of obesity, new report shows
By Kyle Heim
New data released on the economic costs of patients who are overweight or who have obesity in the U.S. shows that Iowa aligns closely with nationwide averages.
The data was shared by Tim Dall, executive director of life sciences at GlobalData PLC, during the Iowa Healthiest State Initiative’s Impact of Obesity on Employers Webinar presented by Eli Lilly and Co. on April 5.
The webinar, along with a Workplace Well-being Conference on April 17 in Ankeny, are the latest efforts by the Initiative to share new data and foster conversations related to people who are overweight or who have obesity, as well as the effects they have on the economy.
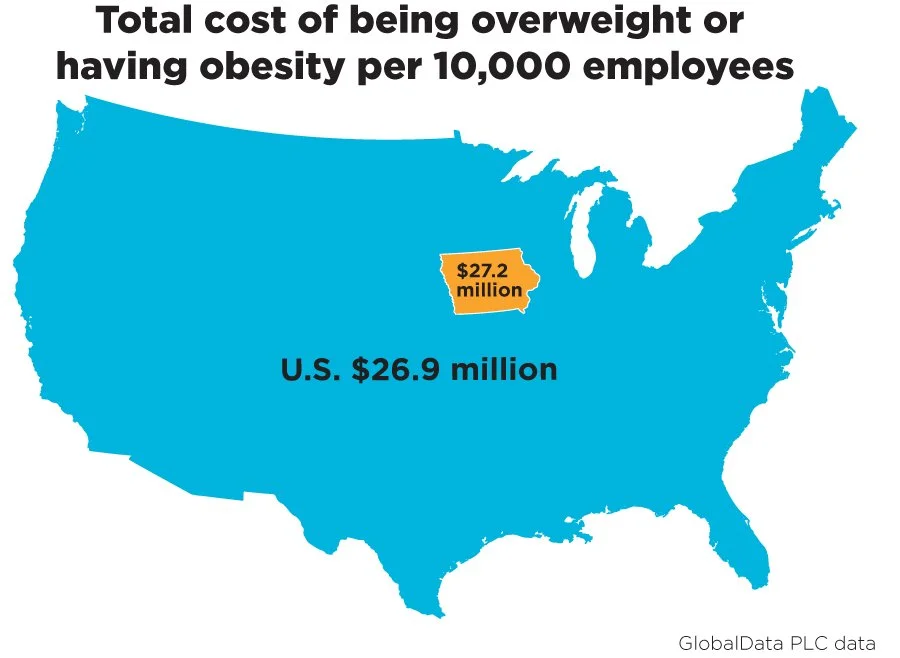
Part of the study included modeling a hypothetical organization with 10,000 employees, in addition to their dependents, and estimating what the cost implications would be for those who are overweight or who have obesity.
“The idea being that if your organization has 20,000 employees, you can take those numbers and double them,” Dall said. “If you’ve got 5,000 employees, you can take the numbers and cut them in half, and that will at least give you a ballpark estimate for what the annual costs are for obesity. I would also note that many of these costs might be jointly borne by the employer and the employee.
“For example, if a person’s productivity is consistently lower because of their health reasons, or if they are consistently missing work because of absenteeism due to health reasons, that might be reflected in lower pay or fewer promotions. And so, employees bear this burden, and also the employer bears part of that burden due [to lost productivity], and some of those are very difficult to quantify.”
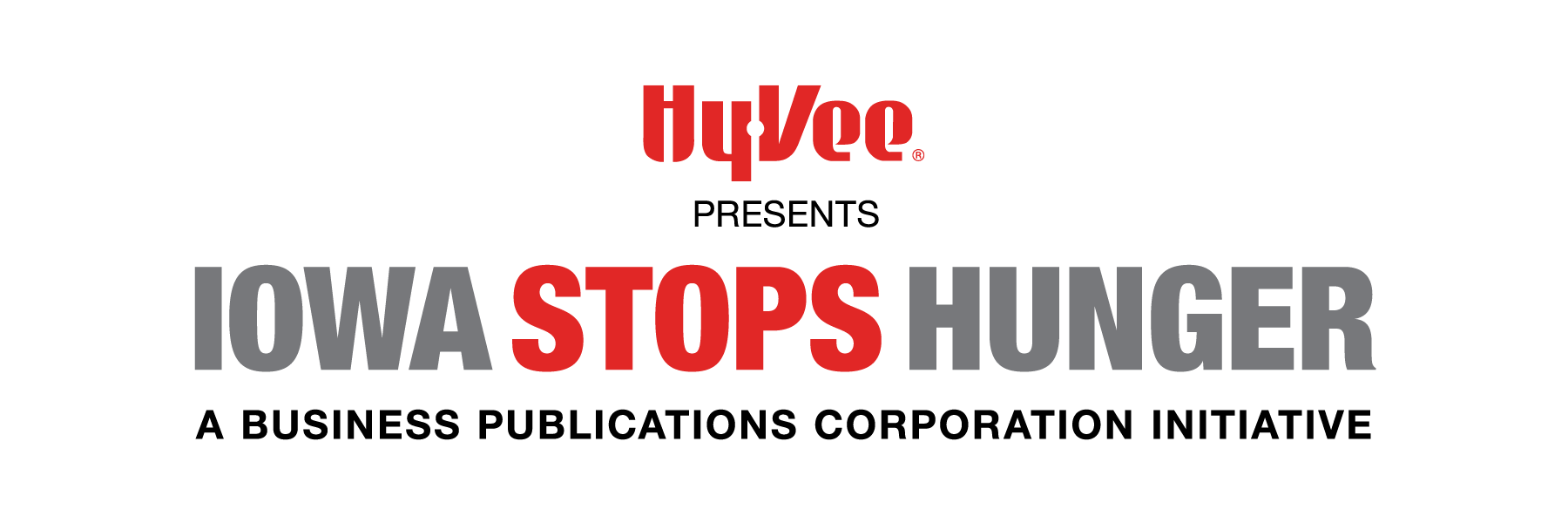
At the national level, the study estimates the cost of being overweight or having obesity for a hypothetical organization with 10,000 employees to be about $26.9 million. For Iowa, the estimated cost is $27.2 million per year for the hypothetical employer with 10,000 employees.
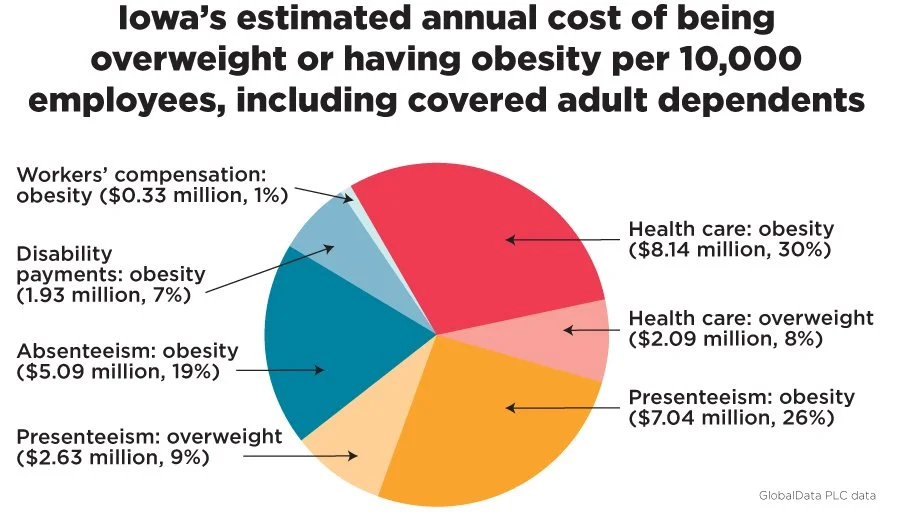
The data also showed that Iowa’s obesity prevalence is about 9% higher than the national average; its overweight prevalence is 1% lower; its cost of living index is 10% lower; and its health care cost index is 1% higher.
In addition to the new data, the study also included a list of recommendations for employers.
The first is to treat obesity like any other disease, such as diabetes or heart disease, and to provide comprehensive insurance coverage for obesity and wellness programs at parity with other chronic conditions.
The second is to upgrade, implement or provide incentives for the use of wellness programs.
“We know that many companies do have wellness programs; there’s always more that can be done,” Dall said. “And in our report, for example, we refer to a diabetes prevention program that’s offered at the worksite that showed an improvement in body weight. So there are wellness programs that can be done and adapted to your workforce.”
The third is to foster a culture of support and inclusion.
“Sometimes this is just making sure that there’s healthy food options if you have a cafeteria or other resources at your place of employment,” Dall said. “Some have gym memberships. It can be things as simple as trying to change the culture, so that if instead of going to a conference room for a meeting like for a one-on-one with a colleague, you might just go for a walk instead.”
The final recommendation is to provide education and resources.
“This involves partnering with your insurance program and other providers just to make sure that employees have the resources that they need,” Dall said. “The idea being that when an employee and their dependents sit down with their health care provider to talk about how they can treat their obesity that they have all the tools available to them to address their obesity.”
A panel including Tracy Sims, executive director of corporate affairs at Eli Lilly and Co.; Megan Jenkins, a patient living with obesity; Dr. Tim Sagers, president of Captive Health; and Dr. Lena Rydberg Freese, an internal medicine specialist at the Iowa Clinic, provided some of their own suggestions and recommendations during the Workplace Well-being Conference on April 17. The moderator was Wes Hartig, CEO of MedOne Pharmacy Benefit Solutions in Dubuque.
“Patients who struggle with obesity are told for years that this is their fault, their problem,” Rydberg Freese said. “There are so many different biases that come out, whether it’s from health care providers, whether it’s from society, it’s all of these things, and people are just bathed in it. And it really limits their ability to move forward.”
Rydberg Freese said that one of the most impactful things employers can do is to act in an empathetic and inclusive way around the body and to consider those things when planning activities, setting up a work environment and educating others.
“I think an employer acting in that way, too, will only help our mission of reducing the stigma,” she said.
One of the biggest challenges Jenkins said she faces is the anxiety she has as it relates to living with obesity.
“Things employers might not think about are what types of activities you are doing for your all-employee events,” she said. “Can everybody physically participate in them? If you’re getting new furniture, I have to think about, ‘Is this chair going to be comfortable? Will I fit in it? Will my body fit in it?’ If I fly somewhere for a meeting, it’s like, ‘Oh, God, is the seat belt going to be long enough for me to fit in it?’ … There is so much anxiety around it. It’s daily, in your face and you’re dealing with it.”
Sims was a co-researcher on a recent in-depth study surveying 1,500 people with obesity, employers and HR leaders.
“It’s interesting, when you look at surveyed employers, the vast majority, over 90% of them, report that they believe obesity is a disease,” Sims said. “But there’s a far smaller percentage who report a willingness to provide access to comprehensive evidence-based care. So, there is a gap, and that gap may be maintained by a perspective on economics [but also likely] maintained due to still existent high degrees of bias and stigma upon the disease.
“Now, interestingly, from the same research, we surveyed over 1,000 people who have obesity, and we asked them, ‘Do you believe that obesity is a disease or that it is more a personal fault?’ And sadly, over 50% of them report it’s a personal fault. To me, this is emblematic of this issue of bias and stigma and the long-standing perspective that we treat obesity simply through eating less and moving more, which we know by and large is not a successful, nor a durable approach for everybody who has obesity.”